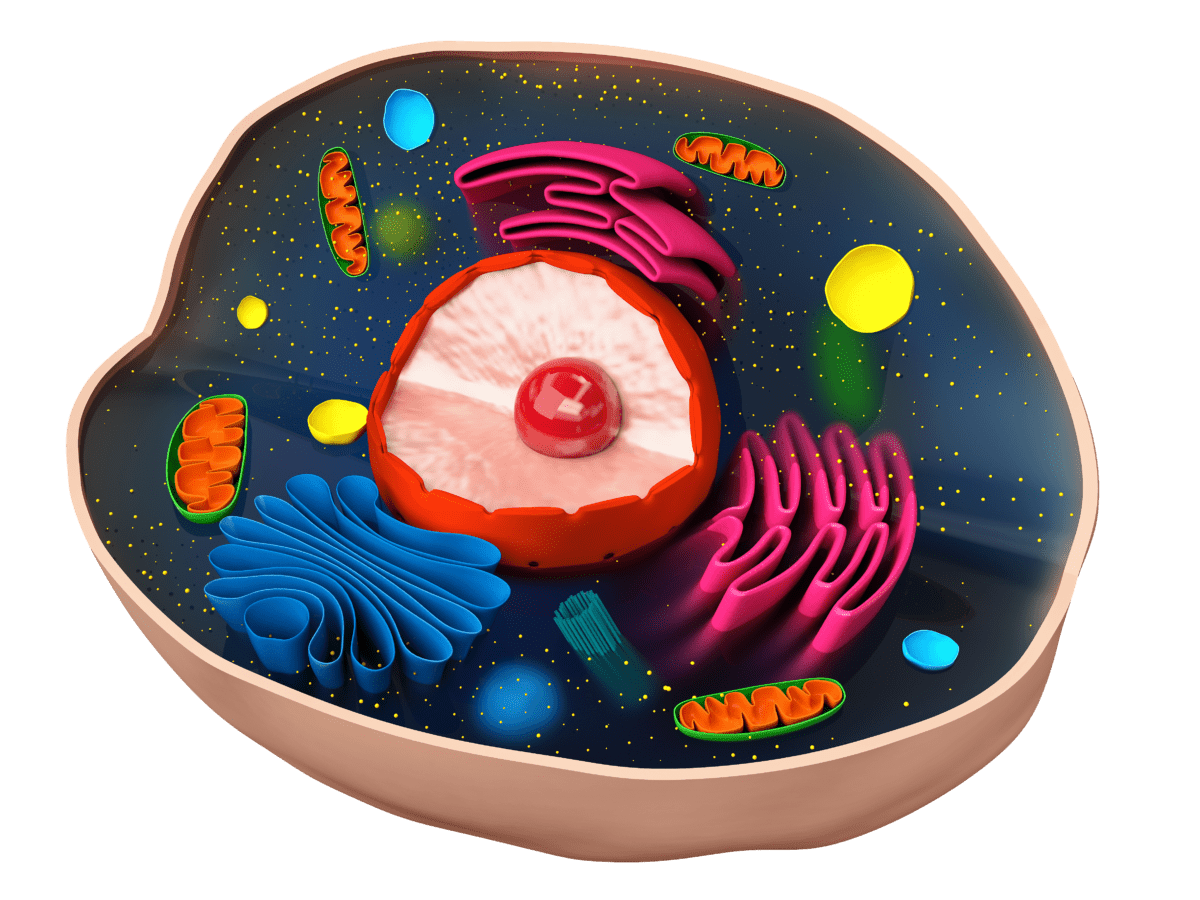
Mucopolysaccharidosis type I (MPS I) is a rare and hereditary metabolic lysosomal storage disease originated by a lack or deficiency of α-L-iduronidase (IDUA) enzyme. The IDUA enzyme is responsible for breaking down complex carbohydrates, known as glycosaminoglycans (GAGs), particularly heparan sulfate and dermatan sulfate. The lack of IDUA in MPS I patients leads to the accumulation of these two GAGs within the lysosomes of the cells. The excess accumulation of these GAGs interferes with proper cell function, affecting multiple parts of the body (Campos et al., 2012; Clarke, 2021; NORD, 2019). There are two types of MPS I depending on the severity of its symptoms: severe MPS I and attenuated MPS I. Severe MPS I, also known as Hurler syndrome, presents early in life (typically diagnosed in babies 6-24 months old) with skeletal abnormalities, arthropathy, coarse facial features, delays in development of motor skills and intelligence, progressive cardiorespiratory complications, enlargement of the head, liver, and spleen, hearing loss, and corneal clouding, leading to death in the first decade of life. Attenuated MPS I presents later in life (typically diagnosed in children aged 3-10 years old) with similar symptoms to severe MPS I but with slower disease progression. Attenuated MPS I patients show variability in their symptoms, some patients have moderate severity, also known as Hurler-Scheie syndrome, and die in the second or third decade of life, while others have mild severity, also known as Scheie syndrome, and have a normal life expectancy (Beck et al., 2014; Clarke, 2021; NORD, 2019). Even though it is difficult to know the exact number of MPS I patients, reports estimate between 200-5,000 patients currently living with MPS I in the US (Puckett et al., 2021).
The treatment of MPS I is limited to hematopoietic stem cell transplantation (HCST), enzyme replacement therapy (ERT), and supportive care. HSCT is a highly invasive non-curative procedure that carries high risk, including 10-15% probability of death. ERT is a good alternative, but there is only one drug FDA-approved in the US, which cannot treat all manifestations of MPS I, particularly the cognitive impairments and abnormal bone development. Supportive care is only used to control the symptoms of the disease as they appear and has no effect on the overall root cause of MPS I (Clarke, 2021; GARD, 2021; Kemper, 2015). Current therapies cannot cure MPS I so there is a significant unmet medical need in this patient population. The development of novel therapeutics to improve the quality of life of MPS I patients and reduce mortality rates is essential.
References:
- Beck, M., Arn, P., Giugliani, R., Muenzer, J., Okuyama, T., Taylor, J., & Fallet, S. (2014). The natural history of MPS I: global perspectives from the MPS I Registry. Genetics in Medicine, 16(10), 759-765. doi:10.1038/gim.2014.25
- Campos, D., & Monaga, M. (2012). Mucopolysaccharidosis type I: current knowledge on its pathophysiological mechanisms. Metab Brain Dis, 27(2), 121-129. doi:10.1007/s11011-012-9302-1
- Clarke, L. A. (2021). Mucopolysaccharidosis Type I. In M. P. Adam, H. H. Ardinger, & R. A. Pagon (Eds.), GeneReviews [Internet]. Seattle (WA): University of Washington, Seattle.
- GARD. (2021). Mucopolysaccharidosis type I. Retrieved 01/18/2022 from https://rarediseases.info.nih.gov/diseases/10335/mucopolysaccharidosis-type-i
- Kemper, A. R. (2015). Newborn screening for mucopolysaccharidosis type 1 (MPS I): A systematic review of evidence, report of final findings (version 1.1). Retrieved from
- NORD. (2019). Mucopolysaccharidosis Type I. Retrieved 01/18/2022 from https://rarediseases.org/rare-diseases/mucopolysaccharidosis-type-i/
- Puckett, Y., Mallorga-Hernández, A., & Montaño, A. M. (2021). Epidemiology of mucopolysaccharidoses (MPS) in United States: challenges and opportunities. Orphanet J Rare Dis, 16(1), 241. doi:10.1186/s13023-021-01880-8
About

Paula Garcia Calavia, Ph.D.
Scientific Officer, BioPharma Global, Inc.
Dr. Paula Garcia Calavia currently functions as Scientific Officer at BioPharma Global (BPG). She has experience in drug development, particularly in medical therapeutics and diagnostics. Her regulatory education includes the completion of a drug discovery, development, and regulation course at UCSF-Stanford Center of Excellence in Regulatory Science and Innovation (CERSI). At BPG, Paula is involved in feasibility and strategy consulting, novel data analysis, authoring expedited approval applications to FDA and EMA, project management, writing pre-IND and IND level submissions to FDA, and preparing clients for Type B FDA meetings. She has worked in diverse projects covering all stages of drug development, from early first-in-human trials to Phase 3 trials, and a variety of indications including oncology, hematology, gastroenterology, immunology, and COVID-19. She is particularly interested in drug development and regulations for rare diseases with unmet medical needs. Prior to joining BPG, Paula worked as a research scientist in R&D towards the development of rapid diagnostic tests for infectious diseases, such as influenza virus and norovirus. Her academic background includes a Master of Chemistry (MChem) in Forensic and Investigative Chemistry, with a focus on drug detection and quantification from fingerprint samples, and a PhD in Cancer Bio-nanotechnology, where she worked in the development of nanoparticles for targeted photodynamic therapy using cancer in vitro models and various nanomaterials, both from the University of East Anglia in the United Kingdom.